BIOE Students Earn Top Honors for Health Innovation at 2025 Capstone Expo
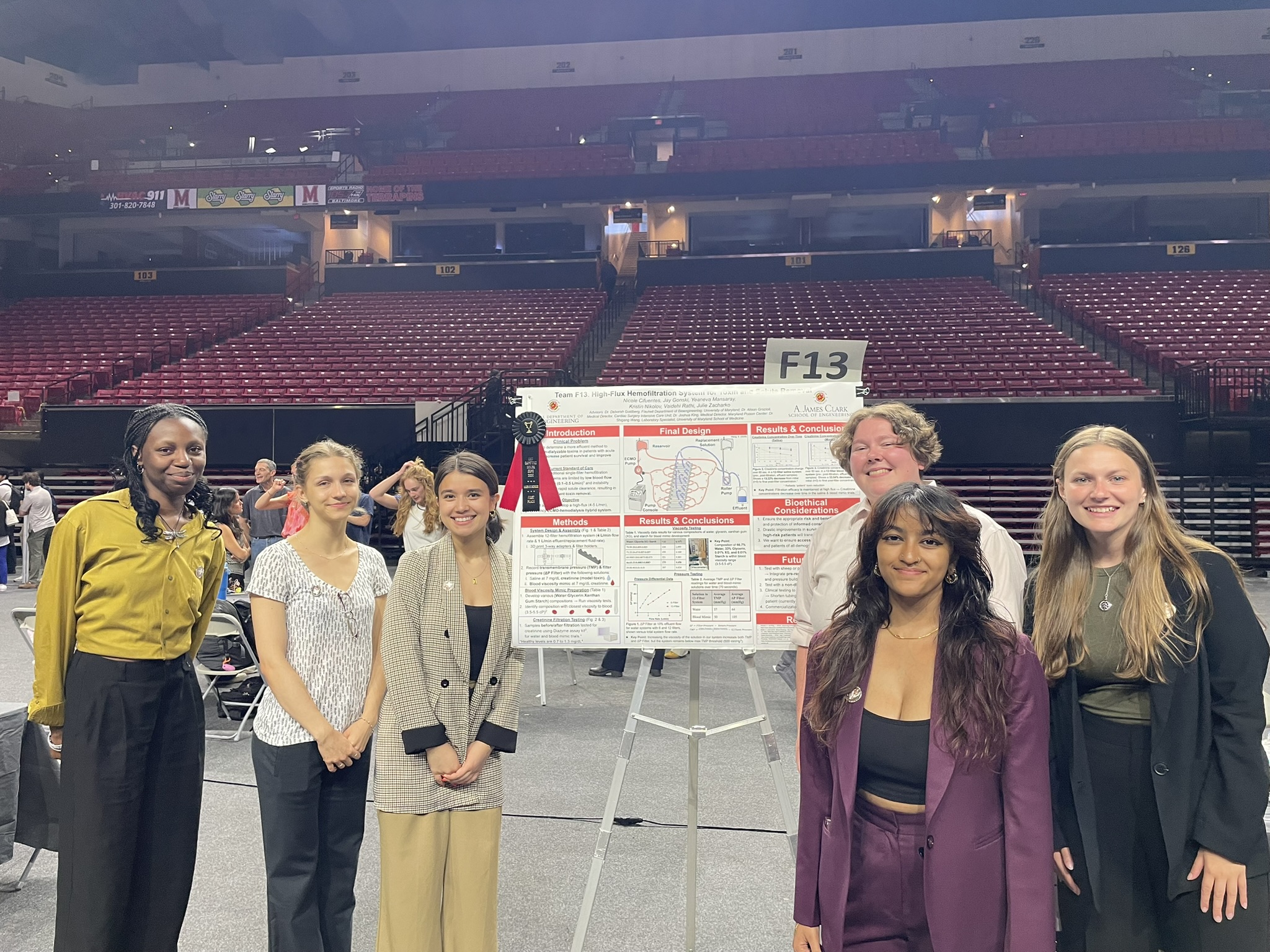
On May 7th, the A. James Clark School of Engineering hosted its second annual Capstone Design Expo, showcasing the ingenuity and hard work of more than 800 engineering seniors from across all engineering disciplines. Held at the University of Maryland’s Xfinity Center, the Expo featured 134 student projects offering solutions to some of society’s most pressing challenges. Students from the Fischell Department of Bioengineering’s bioengineering (BIOE) and biocomputational engineering (BCE) undergraduate programs presented 24 projects focused on advancing healthcare and medical technologies. This year, BIOE teams earned several top honors in recognition of their innovative solutions, including first, second, and third place awards, the department’s Award for Translational Design, and the MPower Award for collaboration. BIOE Team 4 won first place for their project “High-Flux Hemofiltration System for Toxin and Solute Removal.” Current hemofiltration systems don’t always filter blood quickly or effectively, making it hard to remove harmful toxins from the body. To improve this, the team designed a new system using 12 filters that can safely handle higher blood flow. Their system aims to effectively remove toxins, including those historically difficult to filter, and could significantly improve outcomes for critically ill patients. The MPower Award honors exemplary collaboration with the University of Maryland, Baltimore. This award is sponsored by representatives of the University of Maryland MPowering the State Strategic Partnership. The Award for Translational Design, sponsored by the Fischell Department of Bioengineering Advisory Board, recognizes the team with the highest overall design score. Winning teams clearly demonstrate how their design addresses the chosen problem, justify their design decisions and specifications, and present clear diagrams or drawings. This group also earns placement on the BIOE Advisory Board Award for Translational Design trophy, which resides in A. James Clark Hall. The Fischell Department of Bioengineering extends its gratitude to this year’s panel of Capstone judges, including members of the BIOE Advisory Board and esteemed faculty. BIOE’s Capstone Design competition is supported by the Fischell Family, the University of Maryland MPowering the State Strategic Partnership, and Expo event sponsor Whiting-Turner (WT). In addition, BIOE Capstone students benefit from mentorship provided by clinicians and industry representatives, including collaborators from the UMD School of Medicine, Children's National Health System, Becton Dickinson, and the Robert E. Fischell Institute for Biomedical Devices.
Team 1: Bronchoscopic Suture Device Tanya Nikhil Budhiraja, Jonathan Caohuy, Anika Dasgupta, Katriel Kasayan, Duy Le Advisors: Dr. Katharina Maisel / Sponsor: Dr. Chenchen Zhang Bronchopulmonary fistulas (BPF) are a postoperative complication observed after lung surgery in which there is an abnormal connection developed between the bronchial tubes and the pulmonary space. This condition can lead to severe complications and symptoms such as pneumonia, empyema, shortness of breath, and low blood pressure. As a result, there is a clinical need for a novel biomedical device to seal these abnormal openings with minimal trauma to the bronchial tissue. Current treatments for BPFs include surgery and antibiotics to seal the opening, but these introduce risks such as scarring, fibrosis or exacerbated leakage. These fistulas and other conditions of the bronchi are typically examined using a bronchoscope, an instrument consisting of a tube, camera, light, and working channel allowing visualization of and limited interaction with the bronchial tubes. There are two types: The rigid bronchoscope and the flexible bronchoscope. There is a channel within the bronchoscope allowing for the insertion of various surgical tools such as forceps. In our project, we aim to develop a bronchial suturing device that can be compatible with a rigid bronchoscope, and successfully suture fistulas within the bronchial airway. The suturing mechanism is controlled by a wire interfaced with a trigger and consists of a platform actuating a pantograph-like mechanism that bends the staple into the bronchial membrane. To confirm the efficiency of the stapler, chicken breast tissue will be used to simulate the bronchial epithelium in our device testing as it has similar mechanical properties/young’s modulus. Future directions for this project will concern scaling the device down to size and testing so that it may operate in the narrow channel of a rigid bronchoscope.
BCE Team 1:Computer Vision Techniques for the Segmentation and Morphological Analysis of EM Images of the Mouse Hepatitis Virus Pisey Em, Arielle Scott, Christine Vassell Advisor: Dr. Lan Ma This project uses deep learning to analyze electron microscopy (EM) images of Mouse Hepatitis Virus (MHV), a model for coronaviruses, focusing on the structural difference between wild type and mutant variants. Manual segmentation was used to establish ground truth masks, which were then used to train a U-Net model for automatic segmentation as well as a ResNet18 classification model to distinguish the variants. Finally, morphological analysis of spike and body regions revealed consistent differences between the wild type and mutant strains. This pipeline lays the groundwork for future efforts to automatically annotate structural differences in viral morphology, paving the way for studying structure-function relationships in virology, immunology and pathology. Team 2: Head Assessment Tool (HAT) for Improved Monitoring of Infant Head Growth Simon Nikolaos Agritellis, Katelyn Coste, Tova Davidson, Venkata Polavarapu Sarojasamhita Advisors: Dr. Sara Molinari / Sponsor: Dr. Kevin Cleary and Dr. Youssef Kousa, Children's National Hospital Occipital frontal circumference (OFC), or head circumference, is a vital measurement in monitoring child growth and development in infants. An abnormal value can indicate serious health concerns such as micro/macrocephaly and various positional deformities, that lead to significant neurological and developmental complications. The current standard of care for head measurement involves a simple paper measuring tape wrapped around the patient’s head by a physician. This frequently produces inconsistent and inaccurate measurements due to infant movement, and relies upon a single clinical value, potentially leaving some cases of abnormal growth unnoticed. This can result in misdiagnoses, unnecessary medical procedures, and financial burdens for families. (Philadelphia, n.d.). Therefore, a more reliable, repeatable, and user-friendly method is necessary to increase diagnostic accuracy, improve clinical outcomes, and enable accurate brain health monitoring. The proposed solution is a beanie-style cap with colored “markers” placed at significant cranial anatomical landmarks, coupled with a Python image analysis software that computes three critical clinical parameters: OFC, Cranial Index, and Cranial Vault Asymmetry Index. The design has several components, summarized by the major prototyping progress for each: 1) wearable cap, 2) software, 3) the testbed, and 4) the wireframe app. The cap contains raised markers, an embroidered calibration line, and a variable fit. The software analyzes a single image of the top of the head and calculates each clinical value mentioned above. The testbed utilizes a 3D-printed mount platform for seamless integration of a model head into a robotic arm, allowing for testing of the system on a moving subject. A wireframe of the app showcases the device’s potential usability outside of the clinic. The bioethical implications of our system impact three focus groups: parents, patients, and pediatricians. This design is easy to use and allows for more accessible healthcare for both patients and parents. In further clinical applications, data privacy and storage are required as per the Health Insurance Portability and Accountability Act (HIPAA) guidelines. Our system offers medical advice and suggestions but does not eliminate the need for physicians. Rather, it acts as an early warning system to alert patients/parents when treatment may be needed. By enabling early detection of abnormalities, supporting timely intervention, and increasing the likelihood of successful treatments, the device will have a positive impact on infants.
Team 3: Bioengineered Solutions for Enhancing the Longevity of Dental Restorations Elizabeth Everich, Maggie Hampson, Jimena Moreno Chaza, Riya Patel Advisors: Dr. Mueller, Dr. Moore / Clinical Mentor: Dr.Mary Anne S Melo, University of Maryland Medical Center This project seeks to enhance the longevity of dental restorations by addressing the frequent failure of dental composite fillers caused by hydrolytic degradation and bacterial infiltration of Streptococcus mutans and Lactobacillus crispatus. Exposure to moisture, bacterial byproducts, and enzymatic activity compromises the dental filler, often leading to secondary caries and costly, repeated procedures. We developed a resin based composite filler with chitosan (1, 2.5, and 5 wt%) for antibacterial functionality and biofilm inhibition, nanoclay (3 wt%) for improved adhesion and mechanical reinforcement, and polycaprolactone (10 wt%) for mechanical properties and added flexibility. Preliminary prototyping results indicate that at 5 wt% chitosan, the material inhibits Lactobacillus crispatus, while all tested concentrations maintain desired material properties, such as elastic modulus and tensile strength, comparable to commercial fillers. By integrating antimicrobial protection with mechanical durability, this novel antibacterial filler has the potential to reduce restoration failure rates, improve patient outcomes, and offer a sustainable, cost effective solution to one of dentistry’s most persistent problems.
Team 4: High-Flux Hemofiltration System for Toxin and Solute Removal Nicole Cifuentes, Yeaneva Mansaray, Kristin Nikolov, Vaidehi Rathi, Julie Zacharko Advisor: Dr. Goldberg / Clinical Mentor: Dr. Alison Grazioli & Dr. Josh King, University of Maryland Medical Center FIRST PLACE Traditional hemofiltration systems are limited by low blood flow rates (0.1–0.5 L/min) and instability during rapid solute clearance, resulting in inefficient toxin removal. To address these shortcomings, this project aims to develop a high-flux, high-efficiency hemofiltration system capable of operating at significantly higher blood flow rates. Leveraging the Revaclear 300 Dialyzer, we successfully increased flow rates to 4-5 L/min for enhanced clearance. The system incorporates a 12-filter array, each supporting a flux of 500 mL/min, to distribute a total flow of 4–5 L/min while maintaining filter pressure between 100–150 mmHg—crucial for preserving membrane integrity and preventing fouling. This device is also designed to remove a broader range of toxins, including those previously difficult to eliminate. To validate its performance, we tested the system using creatinine as a model toxin and demonstrated its ability to efficiently filter it from circulation. Our team built on proof-of-concept work by University of Maryland bioengineering students to refine the system for clinical application, marking a key milestone in bringing the technology from bench to bedside. Ultimately, this project has the potential to significantly improve outcomes for critically ill patients by expanding access to more effective extracorporeal detoxification.
Team 5: Wearable, Non-Invasive Patient Aspiration Risk Prevention System Ashlyn Casp, Esha Chopra, Dilan Gangar, Mya Hamstra, Matthew Somerville Advisors: Dr. Jeffrey Hasday, Dr. Helim Aranda-Espinoza / Clinical Mentor: Dr. Jeffrey Hasday, University of Maryland School of Medicine Aspiration is a medical condition in which food or liquid unintentionally enters the lungs or airway instead of the esophagus, often causing serious health issues including choking, pneumonia, and chronic lung scarring. A patient can reduce their risk of aspiration by maintaining an upright position during ingestion and rest, but this remains a challenge for many patients experiencing cognitive impairment or limited mobility. The current standard of care requires frequent monitoring from medical professionals or caretakers, but this method is often inadequate given the insufficient patient-to-nurse ratio. To address this unmet clinical need, we developed a wearable, disposable, Bluetooth-compatible device to (1) continuously monitor a patient’s torso angle and (2) notify caretakers when a patient reclines beyond a critical threshold angle. This device can comfortably adhere to the sternum, measure the chest angle using an enclosed accelerometer, store readings in a user-friendly app, and audibly alert the caregiver. Notably, our design is adaptable for both hospital and home settings, offering a non-invasive, sustainable, and accessible solution that accommodates diverse body types. Through continuous, real-time posture monitoring, this device can be implemented in various settings to improve aspiration prevention and patient outcomes.
Team 6: IV Infiltration Detection System for Pediatric Patients Sarah Firdaus, Nida Shah, Vanshika Shah, Tasnim Ullah, Nicholas Varghese Advisor: Dr. John Fisher / Clinical Mentor: Dr. Jason Custer & Dr. Siddhartha Dante, University of Maryland School of Medicine Intravenous (IV) therapy is a critical medical treatment that delivers fluids, medications, and nutrients directly into a patient's bloodstream, typically through a catheter or needle. It is widely employed in hospitals for various purposes, including blood transfusions and the administration of medications. IV infiltration occurs when the fluid or medication intended for intravenous delivery leaks into the surrounding tissue instead of being infused into the vein. This happens when the IV catheter becomes dislodged from the vein or the vein wall is perforated, causing the fluid to escape into the surrounding tissue. Factors such as fragile veins, rapid infusion rates, and using a catheter that is too large for the vein contribute to infiltration. The challenge is particularly significant in pediatric patients, especially infants and young children, who have smaller veins that are also more fragile, and more prone to damage. Due to their limited ability to communicate pain or discomfort, children often cannot alert healthcare providers to issues such as infiltration, which can go unnoticed. If left untreated, IV infiltration can cause serious complications such as tissue necrosis, infections, sepsis, and the need for plastic surgery. The risk of these severe outcomes is heightened because current detection methods rely on nurses checking the IV site every 1-2 hours, which can be time-consuming, delayed, and prone to human error. To address this issue, we developed a device that automatically and continuously monitors IV sites in pediatric patients, providing real-time alerts when infiltration occurs. This not only protects infants and children by reducing harm, improving comfort, and preventing complications associated with IV infiltration, but also spares families the financial and emotional burden that often accompanies these events. Additionally, our device reduces the manual workload for nurses in intensive care units and supports better patient outcomes, which can contribute to improved hospital reputation and quality ratings. Our solution utilizes a flex piezoresistive sensor that detects internal tissue deformation by converting mechanical force—caused by swelling—into changes in analog voltage. As fluid accumulation from IV infiltration increases pressure beneath the skin, the sensor bends slightly, resulting in a measurable rise in voltage. Once this voltage surpasses a defined threshold, the system triggers an audible alert via a buzzer to notify clinical staff. To evaluate the clinical relevance of our device for monitoring IV sites, we drew inspiration from the study “Non-invasive, Multi-Modal Sensing of Skin Stretch and Bioimpedance for Detecting Infiltration during Intravenous Therapy” by Jambulingam et al. (2016), which demonstrated the feasibility of using non-invasive sensing to detect infiltration-related tissue changes. Based on this framework, we conducted preliminary testing using biological tissue models—specifically pork tenderloin and chicken thigh—to simulate soft tissue surrounding an IV site. By placing our sensor on the tissue surface and injecting saline to mimic infiltration, we observed clear changes in analog voltage output from the sensor. In some cases, these changes were sufficient to trigger the buzzer alert. These early results are promising and suggest strong potential for clinical use in pediatric and neonatal care settings. Team 7: Single Step Tracheostomy Device Chelsea Neumann, Tiffany Nguyen, Sidney Redwood, Ritik Saini, Brooke Wunderler Advisors: Dr. Alex Xu & Ryan Smith, Fischell Institute Foundry Engineer / Sponsor: Dr. Joseph Rabin, University of Maryland Medical Center Nearly 100,000 tracheostomies are performed in the United States each year. While this remains an effective method for establishing an alternative airway, patient safety and procedural efficiency continue to be concerns due to the time-consuming, multi-step procedure required by the current standard of care - the Ciaglia Blue Rhino system. Our solution aims to streamline the procedure for surgeons and improve patient outcomes by minimizing procedural complexity, apnea duration, infection risk, damage to the tracheal wall, and tracheal ring fracture. The design features non-compliant concentric balloons over a multi-lumen catheter, enabling controlled, single step, radial dilation. Each balloon inflates independently via separate lumens and stopcock controlled syringes, allowing stepwise expansion with a single insertion. Performance evaluation was conducted through benchtop testing on ex vivo chicken breast tissue, where our prototype successfully created radial deformation and dilation of the artificial tissue, supporting the design’s feasibility. Ethical considerations include ensuring equitable access to the device in resource limited healthcare systems, and selecting safe, biocompatible materials.
Team 8: Agar-Based Lumbar Puncture Training Model with LED Feedback Sa Han, Benjamin Oteri, Brennah Ringling, Audrey Vassia Advisors: Dr. Jenna Mueller / Sponsor: Dr. Kristen Johnson, Children's National Hospital AWARD FOR TRANSLATIONAL DESIGN Lumbar Puncture (LP) is a common medical procedure that involves inserting a needle into the lower part of a patient’s back with the goal of reaching the subarachnoid space and collecting cerebrospinal fluid. The procedure often fails due to low visibility of the area, and can lead to complications such as back pain, spinal hematoma, and damage to nerve roots. There is also limited training to complete this procedure, with the common clinical method being “See one, do one, teach one.” Training devices do exist, but their prices are hefty, with the cheapest technology still costing around $2000. This project explores a way to improve affordability of lumbar puncture training models in low income communities that enhance diagnostic patient care efficacy. This project aims to improve LP success rate through the development of an educational agar ultrasound phantom model simulating the different layers of spinal tissue coupled with a photodiode/LED electronic system, offering visual feedback to clinicians on the spinal layers. The prototype contains a 3D printed model with two main compartments: 1) a section for agar layers, vertebrae, and synthetic skin, and 2) a section that houses the electronics. The agar section contains layers of agar formulations that mimic the stiffnesses and thicknesses of three main layers of spinal tissue: ligamentum flavum, epidural space, and dura mater. 5%, 2%, 7.5 w/v% agarose solutions were determined as corresponding tissue layer upon literature values and relative stiffness, which were determined through compression testing. The vertebrae are placed in the center of the agar to emulate realistic experience of lumbar puncture. The user will engage with a custom-built needle with an LED in the tip to interface with photodiodes mounted at the bottom of the agar tissue. The electronics compartment houses the circuit and Arduino Uno microcontroller that takes in light intensity values from photodiodes. As the needle tip travels downward through the layers, a labeled red LED will turn on, indicating to the user that their needle has passed through. This process will continue for all three layers mentioned above. This circuit will provide real time feedback for the user to fully understand and learn what each of the layers should feel like as the needle tip passes through the tissue. Overall, this physiologically relevant educational tool will provide more hands-on practice for clinicians performing lumbar punctures and lead to more success when the procedure is conducted on a human patient. Benefits of increased practice and increased success rate include increased patient safety, minimizing the aforementioned complications associated with failed LPs. Healthcare providers benefit as they have more practice of doing the lumbar puncture without needing a patient to do it, increasing practice affordability for lower income hospitals. Patients benefit from reduced physical and psychological harm which can overall increase their safety. In addition, for children and patients who have a fear of needles, this can increase their comfort of the procedure.
Team 9: Updated Central Venous Catheter Guidewire Management Device Yeabsira Belay, Calvin Le, Brooke Marchesi, Camila Govanna Rivera, Megan Tran Advisors: Dr. Walter Banfield, Dr. Huang Chiao, Dr. Robert Dunn, Dr. Kyle Glose, Dr. Matthew Grzywinski / Clinical Mentor: Dr. Matthew Grzywinski, Dr. Walter Banfield, Dr.Robert Dunn, Dr. Kyle Glose The Central Venous Catheter (CVC) is a critical medical device used to deliver fluids, medications, or blood into a patient’s central veins, such as the internal jugular vein, using the Seldinger technique. This method uses a J-shaped guidewire to reduce the risk of inadvertent vessel injury. However, in high-pressure clinical environments, specifically in emergency settings, clinicians often face challenges reinserting the guidewire into the small diameter of the tip, then back into the advancer and sheath after withdrawal. The guidewire may become coated in blood and ultrasound gel, making it difficult to manipulate and reinsert. This can lead to the bending of the wire, increasing the risk of procedural delays, additional medical waste from opening a new CVC kit, and potential harm to the patient.
This project aims to address these technical difficulties and improve reinsertion efficiency by altering the current design of the guidewire management device. Our solution features an expandable, split body design with a snap-clip mechanism that when pulled back, allows the two halves to open and expose the wider diameter of the advancer. The two halves can be reunited by pinching, or forcing, the clip together again, in a snapping manner. The two halves are connected by a curved connector that is bendable and allows precise re-alignment. The protruding piece serves as another alignment and closing feature, such that the device must align to close as the wedge piece fits into the corresponding cavity. An additional adjustment to the tip is making the walls thicker, which reduces misalignments or gaps and ensures structural integrity. With this, we also made adjustments to the advancer, expanding its inner diameter from 2 millimeters to 4.5 millimeters at the point of attachment to the tip, while maintaining the remainder of the original design to maintain compatibility with the existing CVC procedures.
The prototype was developed using SolidWorks and evaluated through Finite Element Analysis (FEA) to ensure structural integrity. The CAD-based designs were 3D printed at Terrapin Works and have undergone usability testing with our clinical mentors at the University of Maryland Medical Center’s Trauma Simulation Lab. Testing compared reinsertion time, ease of use, and reliability under realistic conditions. By integrating clinician feedback and iterative prototyping, this device seeks to reduce procedural complications, enhance clinician performance, and ultimately improve patient outcomes during CVC placement.
Team 10: Preventing Deaths by Opioid Overdose: What if Addicts Were Never Using Alone? Joel Bannerman, Matthew Ensign, Jander Kugelman, Emily Passaro, Peter Shin Advisors: Dr. Catherine Kuo / Clinical Mentor: Dr. Terry Dean, University of Maryland Medical Center The ongoing opioid crisis has highlighted the urgent need for rapid, life-saving overdose interventions. This project aims to address this by developing an automated device capable of detecting opioid overdoses in real time and administering naloxone to reverse the overdose. The system combines real-time monitoring of heart rate, blood oxygen concentration, and rate of carbon dioxide expulsion to determine when an overdose occurs. If these measurements reach critical threshold values, the device triggers an automatic subcutaneous injection of naloxone to reverse the overdose before emergency services arrive. The device is designed for ease-of-use and accuracy, and aims to reduce opioid-related fatalities by ensuring timely intervention when there are no bystanders to administer naloxone. Our approach combines biomedical engineering, real-time monitoring algorithms, and automated drug delivery mechanisms, offering a promising tool in the fight against the opioid crisis. Our pulse oximeter was accurate within 1 bpm of the industry standard ROSCOE pulse oximeter. When deprived of input from the sensors, simulating an overdose, the delivery method was enacted and our alarm was triggered.
Team 11: Developing Automatic Inverting Solution to Mitigate the Effects of Preanalytical Error on Blood Samples Dalton Hass, Aidan Kirby, Emilia Pedreros, Abby Rosenberg, Nitya Venkatiahgari Advisor: Dr. Alisa Morss Clyne / Clinical Mentor: Dr. Terry Dean, Children's National Hospital The goal of this project is the development of a novel device to limit blood sample quality error. To begin, we first wanted to identify what a blood sample quality error was and what caused them. We dove into research regarding the total testing process, techniques applied in blood sampling, examples of blood sample quality errors, data collection for causes of blood sample rejection, and the effect of sample rejection on healthcare costs and patient experience. We found that most errors occur in the pre-analytical phase of blood testing. This is due to the manual labor required for blood sampling. The best way to prevent pre-analytical errors is to improve lab procedure. While this may be a great solution in a low stakes diagnostic setting, unfortunately in the busy healthcare setting this solution is not very feasible. We also identified that some of the main causes for sample rejection were, in the following order of frequency, insufficient sample, clotted sample, incorrect tube, and hemolyzed sample. This inspired us to look further into the cause of these rejections and we came up with three design ideas to address these issues: an automatic detector of improper sample size, a temperature controlled storage casing, and an automatic inverter of sample tubes.
We believe that if a casing were to automatically determine if the sample is over or under filled, the sample could be redrawn faster, which would limit the delay between when the error is discovered and when the sample is redrawn. We also speculate that if samples are held at consistent temperatures, then quality would improve. Additionally, we presume that proper mixing of the sample would result in less error as well. We found that oftentimes the sample tubes are improperly mixed, meaning additives in the tube required for further testing or to prevent clotting are not properly incorporated into the blood. Most tubes must be inverted 5-10 times based on the additives in the tube and eventual test performed. After considering these options, we decided to move forward with the automatic inverter design. We found that there were no designs or patents on the market that provided complete inversions based on the requirements of the sample tube. We identified the tube roller and tube rocker, which gently roll and rock tubes continuously, but do not perform total inversions or even identify the sample tubes appropriately.
Our design consists of a chassis that houses an electronics component as well as a rotary housing component that houses six BD Vacutainer® blood vials. Photosensors and a MATLAB algorithm detect and sort the samples to calculate the amount of inversions necessary. The proposed design will be automatic, user-friendly, and accurate. We also began planning our experiments to test the effectiveness of our device. These experiments will utilize animal blood and a variety of tubes to see if the device limits sample quality error. We believe the device will reduce hospital costs and improve patient experience, while easing the workload of healthcare workers everywhere.
Team 12: Self-Expanding Cannula with Small Incision for Mechanical Circulatory Support Alaya Chubb, Jason Costa, Christopher Guerra, Rishika Jadhav, Trixy Tran Advisors: Dr. Kimberly Stroka / Sponsor: Dr. Dong Han, University of Maryland School of Medicine Heart and lung diseases, namely Adult Respiratory Distress Syndrome (ARDS) and trauma-related hemorrhage, are the leading causes of death in the United States. Heart failure affects approximately 6.2 million people, with lung disease accounting for 1 in 6 deaths yearly. Mechanical circulatory support (MCS) is critical to manage these diseases, and is commonly achieved through Ventricular Assist Devices (VAD) or extracorporeal membrane oxygenation (ECMO). MCS system deployment is highly invasive and can result in various complications, including bleeding from the heart, corporeal trauma, delayed incision site healing, and postponed resuscitation. These procedures require skilled surgeons, which is problematic under emergency circumstances. There is an urgent need for a minimally-invasive, rapidly deployable cannula system that simplifies MCS procedures, reduces tissue trauma, and mitigates cannula failures, thereby expanding access to life-saving treatments. We sought to develop a novel cannulation device that is inserted at a minimal diameter and utilizes a peripheral dilation balloon for rapid deployment. Throughout the prototyping phase, we were able to select an adequate tubing, choose a complimentary dilatation balloon, and test its ex-vivo performance. Our design aims to improve access to timely life-saving care, enhance patient recovery, cannula site healing, and quality of life post-operation.
Team 13: Development of a Device to Measure Pressure Waves Along the Infant Tongue During Bottle Feeding Casey Byrne, Veronica Mertz, Caroline Miller, Talya Simcox Advisors: Dr. Nancy Bauman, Dr. Kyung Koh / Sponsor: Dr. Nancy Bauman, National Children's Hospital Mothers all around the world give birth to children with the goal of breastfeeding their child. Unfortunately, not all mothers and babies are able to successfully breastfeed due to multiple causes. One of the more common blocks to breastfeeding is a condition known as ankyloglossia, it causes pain or prevents breastfeeding altogether. This is a disorder in which the tissue that connects the tongue to the floor of the mouth limits tongue mobility. It is also known as “tethered tongue” and occurs in about 8% of newborn babies and about 50% of these babies have difficulty breastfeeding. A very common procedure that is used to reverse the tongue tie is called frenectomy, the clipping of tongue tie, the doctor simply cuts the part of the tongue connecting it to the bottom of the mouth. In successful cases, a frenectomy can lead to the mother being able to comfortably breastfeed. However, in lots of cases, the procedure does not change the outcome of the mother being able to breastfeed. The question then becomes, why does frenectomy fail in some babies, but they can still drink from a bottle without difficulty? This area of research is not very well understood and varies extremely from case to case. One aspect that is known is that there is tongue movement and sequential pressure changes along the entire tongue during the feeding process. By making a device that records the dynamic changes along the entire tongue surface as the baby is feeding, researchers may be able to predict the effect of the frenectomy and avoid having to perform an unnecessary procedure. If successful, this device will improve the understanding of breastfeeding and bottle feeding, enable controlled studies on assessing the outcome of frenectomy, and improve predictions on what patients would actually benefit from the procedure.
Team 14: Patient Safety Monitoring System Zaki Chowdhury, Dylan Dossou, McKenzie Rowe, Emily Thompson, Karen Zhao Advisors: Dr. Guiliano Scarcelli / Sponsor: Dr. Jeffrey D. Hasday, University of Maryland School of Medicine In hospital settings, patients often depend on multiple medical devices to aid in their treatment and recovery. A persistent challenge faced by healthcare providers is the unintentional removal of critical medical tubes, most notably endotracheal tubes, by agitated or disoriented patients. Such self-extubation events can result in serious complications and are typically addressed through physical or pharmacological restraints. However, these interventions raise ethical concerns, including increased patient distress, higher risk of complications, and reduced overall comfort. There is a need for a solution that enables early detection of risky patient behavior without compromising patient comfort. To address this, we propose a non-intrusive, real-time video-based monitoring system designed to enhance patient safety by accurately detecting dangerous movements and issuing immediate alerts to healthcare staff. Our prototype consists of two USB webcams connected to a Raspberry Pi 5, running Python in combination with Mediapipe and OpenCV for real-time image analysis and object tracking. Colored markers are strategically placed on medical tubing to monitor their spatial relationship. If the distance between these markers falls below a threshold, suggesting a risk of tube dislodgement, the system activates an alarm to prompt intervention. The system carries positive ethical implications for patients, healthcare providers, hospitals, and AI technology companies. By reducing self-extubation incidents, it can lead to better patient outcomes and lower costs related to prolonged ICU stays. However, its use of surveillance will require careful consideration of data privacy and security standards, including strict adherence to HIPAA regulations.
Team 15: A Rapid and Sensitive Cognitive Assessment Instrument for Delirium Ruth Efrem, Jeffrey Luo, Furqaan Nadeem, Sanjith Narayanan Advisors: Dr. Beatrice Kondo / Clinical Mentor: Dr. Cha-Min Tang, University of Maryland School of Medicine Delirium, a frequently misdiagnosed condition affecting up to 35% of hospitalized patients, is associated with increased risks of cognitive decline, extended hospital stays, and mortality. Standard delirium assessments are given manually, take considerable time and resources, and do not quantify cognitive fluctuations, a key indicator of delirium. This project aims to develop a rapid, digital cognitive assessment tool optimized for frequent and standardized use in clinical settings. Our tablet-based application measures patient performance in key cognitive domains, including attention, orientation, and sequence memory through short, interactive tasks. In early testing with non-delirious participants, the tool demonstrated competitive completion times (1 minute 33 seconds) compared to the 3D-CAM (1 minute 54 seconds), alongside promising sensitivity in detecting cognitive changes. Key design features, including quantitative scoring, audio guidance, and an accessible user interface, were implemented based on user and clinician feedback. While initial testing has shown encouraging outcomes, further validation in clinically relevant populations is underway. Ethically, this tool promotes equitable cognitive assessment by being accessible, non-invasive, and easy to administer across diverse patient populations. Ultimately, our solution aims to provide clinicians with a quantitative and robust tool to facilitate delirium detection, increase efficiency, and improve clinical outcomes for vulnerable patients.
Team 16: Fluid-Filled Cuff to Measure Diastolic Blood Pressure During CPR Basim Ahmed, Ishmam Tausif Ahmed, Sidhant Narula, Elisa Pierpaoli, Gahl Shem-Tov Advisors: Dr. Edward Eisenstein, Sponsor: Dr. Michael Shoykhet, Children's National Hospital Our goal is to develop a non-invasive device that EMTs can use that can continuously measure diastolic blood pressure while performing compressions. There are various parts of the project that we can focus on, which are the prototyping of a flat cuff that can be filled with fluid, testing and optimizing the current prototype already developed by Dr. Shoykhet and his team, and modeling the propagation of waves through the cuff and on the pressure sensor. Key features include the utilization of water for faster, more accurate measurements, the ability to measure pressure during both inflation and deflation, low compliance due to the non-compressible nature of the fluid, and a feedback loop system incorporating pressure sensors and a piston mechanism.
Team 17: Match4Life - An App for Optimal Donor-Recipient Size Matching in Thoracic Organ Transplants Shoshana Distenfeld, Heather Horowitz, Theodore Mushiang Hsiao, Sean Judge, Isabelle Kenga Ngassa Advisors: Dr. Yang Tao / Sponsor: Robert M. Reed and Michael H. Eberlein, University of Maryland School of Medicine MPOWER AWARD In thoracic organ transplantation, inaccurate donor-recipient size matching can result in serious complications and poor patient outcomes. Existing matching methods rely on basic metrics like height and weight, which often overlook critical anatomical differences attributed to age and sex. Match4Life is a mobile application developed to modernize this process using evidence-based calculations for predicted Total Lung Capacity (pTLC) and predicted Heart Mass (pHM). The beta version of the app, currently undergoing clinical testing, enables physicians to input patient data and receive accurate match ratios and risk assessments in under ten seconds. Built using Flutter and tested on both iOS and Android platforms, it significantly streamlines decision-making compared to more traditional workflows. The latest, or more advanced version, now includes a secure login, patient data storage, and automated match recommendations tailored to clinical priorities. Match4Life has the potential to become a widely adopted tool, making the organ matching process faster, safer, and more patient-centered.
Team 18: Specialized Aerosolization Catheter for use within Rndotracheal Tube. Tsega Abebe, Kristen Bradish, Trinidad Cubillos Valdes, Julia Fitlin, Claire Kettula Advisors: Dr. Greg Duncan / Clinical Mentor: Dr. Jeffrey Hasday & Dr. Richard Dalby, University of Maryland School of Medicine SECOND PLACE The current method for delivering inhaled medication to intubated patients involves using a nebulizer or inhaler at the top of the endotracheal tube (ETT). Current practice is to introduce aerosolized medications at the proximal end of the ETT. However, due to ETT dimensions and turbulent flow within the ETT, delivery of medications to the lungs is inefficient and unpredictable. Accurate distribution of the medicine is crucial for patients in critical condition. This clinical need has led to the formulation of a method to generate the therapeutic aerosol at the distal tip of the ETT, reducing medicine loss within the tube. Our project is creating a double-lumen catheter that accommodates an aerosol head that will be threaded through to deliver the medication closer to the bronchi. The aerosol head has a specified mechanism that creates particles between 5-10 microns in size. Our current prototype can successfully deliver 89.3% of administered medication at the distal end with some particles being between 5-10 µm. Our device will positively impact health care staff, patients, and their families by increasing medication delivery and improving care outcomes. Hospital administrators will also benefit due to the device’s low cost per unit and low medication waste as well as easy set up and predictable delivery of the medication to the lungs.
Team 19: Endobronchial Blocker Kaylin Baumiller, Marsh Hessler, Kevin Le, Ramadan Mobarek, Mikaela Truong Advisors: Dr. Jenna Mueller; Dr. Xiaoming He / Clinical Mentor: Dr. Faria Taj & Dr. Ashutosh Sachdeva, University of Maryland Medical Center Management of massive hemoptysis following a transbronchial needle biopsy presents significant clinical challenges in healthcare due to a lack of transbronchial or tertiary bronchial blockers. Current solutions on the market, such as the Arndt endobronchial blocker, are too large to fit in the transbronchial space and do not remain deployed for the ideal amount of time to cause thrombogenicity behind the blocker, risking continuous bleeding from the location of the biopsy. We have designed and conducted preliminary testing of blockage device prototypes that can be inserted into the transbronchial and tertiary bronchi using a standard therapeutic bronchoscope and remain deployed beyond the time required for blood to clot. We have confirmed the general shape of our design via large-scale prototypes, identified and tested deployment and extraction methods, and laid the foundational work in the blockage material. We have also established methods to test our prototype in more representative environments, including cadaver studies and an in vivo model. This device enables physicians to treat hemoptysis in patients who receive a needle biopsy in a non-invasive procedure more efficiently, without the need for an operating room, reducing cost, time, and patient stress. Most importantly, it allows for targeted treatment at deeper bronchial levels which evades the need to block off an entire lobe of the lung and reduces respiratory burden on unaffected lung tissue.
Team 20: Smart Inhaler Benjamin Canada, Michael Mankowitz, Jacob Sapin,Isaac Thomas Advisor: Dr. Steven M. Jay / Clinical Mentor: Kevin Cleary, Children's National Hospital Asthma is a chronic respiratory disease that affects over 27 million people in the US, with 10 people dying daily. Most of these deaths are completely preventable, but due to the complicated process of administering medication through inhalers, patients fail to receive proper care. Conventional devices like Metered Dose Inhalers (MDIs), Dry Powder Inhalers (DPIs), and Nebulizers require precise technique and posture, yet 94% of patients report incorrect usage. To address this, we developed an MDI-canister-compatible smart inhaler capable of delivering asthma medication more effectively by automating the administration process. Our prototype senses lip placement, posture, inhalation/exhalation flow, and the number of canister shakes, then actuates medication release when optimal conditions are met. The medication is only administered once inhalation is sensed (breath actuated) and the user lifts the cap lever. This enhances usability and promotes correct administration. By improving patient outcomes and reducing hospital visits, the device can free up clinical resources. While upfront costs may raise concerns about health equity, they may be offset by reductions in long-term care expenses, offering an overall ethical and practical benefit.
Team 21: Automating the Elience™ PoC System Arjun Gupta, Akhil Jayan, Alexandria Slokan, Daniel Michael Tullier Advisors: Dr. Bentley, Dr. White / Sponsor: BD: Andrew Beamesderfer, Kelsey Graves, Andre Scherz Infectious diseases present a significant global health challenge, leading to millions of deaths annually. Many current diagnostic methods are labor-intensive, costly, and slow, creating barriers to timely treatment. Point of Care (PoC) Devices can solve many of these issues, but they need to be automatic and not require manual intervention from the user to be an effective alternative. This project involves the automation of the BD Elience™ PoC device. The Elience™ system consists of a patient sample loaded in a container called the consumable. The consumable is then closed with a transport cap and loaded into the tabletop Elience™ diagnostic device. After a subsequent heating step, the transport cap must be manually switched with the dispense cap and attached piston. The piston pierces through the consumable, allowing the patient sample and chemical reagents to mix, which the device can then read. The goal of this project is to develop an accessory device to automate the process of cap transfer within the Elience™ diagnostic device. Our design incorporates three linear actuators (one horizontal and two vertical) that will be used to position a stepper motor-powered claw mechanism to twist off the transport cap and twist on the dispense cap. Our mechanical prototype is cost-effective and utilizes commercially available electronic components to make the device easy to produce. The prototype is self-powered and effectively utilizes independent actuators to perform the cap transfer and create the appropriate torque. The device will be readily available in clinics and labs, enabling public access to the device and test. The automation will benefit patients and clinicians with faster diagnoses, enabling quicker treatments and reducing the spread of disease.
Team 22: Low-Cost Increased Accuracy Pulse Oximeter For People With a Darker Skin Complexion David Deguzman, Mehul Donthi, Edward Joseph Dorsie, Ananthakrishnan Nair, Laena Nho Advisors: Dr. Adrian Holloway, Dr. Siddhartha Dante / Sponsor: Dr. Brian Blair THIRD PLACE Pulse oximeters are popular devices that measure oxygen saturation levels to monitor respiratory function through determining the oxygen saturation of a patient’s blood. However, this medical device has been shown to overestimate oxygen levels for patients with darker skin inaccurately. Clinical standard pulse oximeters rely on light absorption through the skin to measure blood oxygen saturation, and due to this mechanism, they tend to provide less accurate readings for people with darker skin tones due to higher melanin interfering with light absorption. This issue is also compounded with the high cost of pulse oximeters, making them inaccessible in low-resource areas. The project focuses on designing and developing a low-cost pulse oximetry for children with darker skin, allowing for more accurate detection of critical congenital heart disease (CCHD) in developing communities. This innovative device will quantify the patient’s skin tone with a melanin quantification system. After the patient’s skin tone is quantified, our correction factor algorithm will take into account a patient’s skin color metric and apply a respective correction factor to the original blood oxygen saturation reading. This correction factor will modify the live measurement allowing for a more accurate measurement to be displayed. This work will contribute to more equitable healthcare outcomes by improving diagnosis accuracy for individuals with darker skin tones, particularly in low-resource settings.
Team 23: Artificial Intelligence Tool for Hirschsprung's Disease Diagnosis Anirudh Addepalli, Ilana Borison, Jacob Sandler, Satya Shah Advisors: Dr. Silvina Matysiak / Clinical Mentor: Dr. Marc Levitt, Childrens National Hirschsprung’s Disease, a congenital condition affecting 1 in 5000 newborns, is diagnosed through the detection of ganglion cells in rectal biopsy slides – a time consuming process traditionally reliant on expert pathologists. To address this, our team developed an AI-powered diagnostic tool that uses a convolutional neural network to automatically identify ganglion cells from biopsy images. Integrated into a user-friendly web application, the tool allows clinicians to upload slides and receive quick diagnostic results. Through iterative prototyping, we found that 256x256 grayscale image tiles paired with a large neural network and 50 training epochs produced the highest recall for detecting Hirschsprung’s Disease. Ethically, our solution promotes global healthcare access and diagnostic efficiency, though it necessitates careful mitigation of potential biases and over-reliance on AI to prevent misdiagnosis.
Related Articles: May 20, 2025 Prev Next |